Definition – Mental illness, also called mental health disorders or conditions, refers to a wide range of mental health conditions — disorders that affect your mood, thinking, your perception of reality and your behaviour and conduct. Examples of mental illness include Depression, Anxiety disorders, Schizophrenia, eating disorders, addictive behaviours and Borderline Personality Disorder.
What Is A Dual Diagnosis?
Many people diagnosed with a substance use disorder (an addiction) also suffer from a co-occurring mental health or behavioural disorders. This is known as a “dual diagnosis”. Individuals with a dual diagnosis require an integrated treatment plan that addresses both disorders as interconnected health issues simultaneously. According to a recent study, approximately 80% people with an addiction also have one or more co-occurring mental health conditions among other physical health conditions too.
By seeking treatment for addiction and a co-occurring behavioural or mental health condition, you will stand the best chances of successfully attaining the fulfilling, healthy, substance free lifestyle that you do deserve, however are denying yourself of at the moment!
Does The Medical Community Recognise Alcohol & Drug Addiction As A Disease?
Yes! Since 1956, the UK has identified substance addiction as a health disorder characterised by compulsive decision-making, impulsive behaviours, relapse(s) along with self-destructive and risky behaviours. This disease theory of substance addiction is based on the following criteria:
- Biological in nature (illness exists in and of itself)
- Does not go away or heal on its own without treatment or therapy
- Exhibits observable signs or symptoms
- Is progressive (can and will get worse, even fatal if left untreated)
- Has a predictable timeline of development and recovery
- Often have similar reasons with others as to why they became addicted
- Have similar thinking strategies that are self-destructive
- Physical evidence of negative & destructive behaviours and actions around family, friends, colleagues, healthcare professionals, criminal justice staff and others
In 1956, the National Health Service (NHS) identified substance use disorder as one of a number of primary mental health disorders that also have an associated co-occurring health conditions.
How Did History See Drug & Alcohol Addiction?
In the sixteenth century, alcohol (called “spirits”) was used largely for medicinal purposes. At the beginning of the eighteenth century, the British parliament passed a law encouraging the use of grain for distilling spirits. Cheap spirits flooded the market and reached a peak in the mid-eighteenth century. In Britain, gin consumption reached 18 million gallons and alcoholism became widespread.
The nineteenth century brought a change in attitudes and the temperance movement began promoting the moderate use of alcohol—which ultimately became a push for total prohibition.
You can view a timeline here, explaining how drug and alcohol addiction has been viewed throughout our past few decades. You can find Drugwise timeline here. You can also download it from our downloads & media page here.
In What Way Is Addiction A Mental Health Condition?
Like depression and other mental health conditions, addiction is a very real medical disorder that is rooted in genuine chemical and physical changes in the brain, but the condition is so much more complex than that. According to the NHS “Addiction is a primary, chronic disease of brain chemicals, structure, reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations that present themselves in active substance addiction. This is reflected in an individual pathologically pursuing rewards and/or relief by substance use and other addictive behaviours”.
The past president of ASAM, Michael Miller, explained it this way: “At its core, addiction isn’t just a social problem or a moral problem, failing, laziness or simply a criminal problem. It’s a brain problem whose behaviours manifest in all these other areas. Many behaviours driven by addiction are real problems and sometimes criminal acts do become involved too. But the disease of addiction is about brains, not drugs or alcohol. It’s about the underlying neurology, not outward actions.”
Mental and emotional symptoms occur long before physical symptoms appear. If behavioural and/or mental symptoms aren’t appropriately treated, long-term drug and/or alcohol use can lead to physical complications such as cirrhosis of the liver, chronic brain deterioration, loss of memory, taking dangerous risks that they wouldn’t otherwise have done, infections, cancer and, the most serious consequence of all, coma and/or death.
The Disease Model Of Addiction Explained
Addiction is a disease related to the brain. It is recognised as a chronic disease that must be treated, managed and monitored over a person’s lifetime. Addiction involves changes in the functioning of the brain and body. The disease theory of addiction defines addiction as a compulsive disorder that occurs due to chemical and physical changes in the brain, which is induced by regular use/abuse of drugs and alcohol rather than a conscious decision.
The Disease Model Of Addiction & Defining Addiction
The disease model of addiction focuses on a user’s loss of control, which is primarily caused by substance use (both drugs and alcohol). It suggests that addicts don’t have the ability to discontinue their substance use on their own without the appropriate treatment, therapies and coping tools and strategies. The disease model of addiction states that addiction is a relapsing and chronic brain disorder, with rates or relapse at around 40% to 60%, similar to relapse rates of other chronic medical conditions such as diabetes, hypertension and asthma.
What Are The Sources Of Addiction In The Disease Model?
The traditional medicinal model of disease only requires the presence of an abnormal condition that induces distress, discomfort or dysfunction to the affected person. However, the contemporary medicinal model states that addiction occurs due to changes in the mesolimbic pathway in the brain. It also addresses the fact that such disease may be influenced by other sociological, psychological or biological factors, even though the mechanisms of these factors are not completely understood. Using the contemporary medicinal model for addiction was categorised as a disease is how nearly all treatment providers, therapists and researchers see to treat and arrest active addiction, promote recovery through abstinence and active efforts to remain in recovery.
The disease model of addiction describes an addiction as a disease with environmental, genetic, neurological and biological sources of origin, all of which play an important role in who becomes an addict and what needs to be done to treat an addicts addiction through therapy, counselling and others who can help heal the emotional and mental damage many addicts often receive and struggle to cope with throughout their life without help.
Biological Sources Of Addiction
This suggests that a person’s unique physiology (the way their body works) can contribute to addiction. Some people may enjoy a substance so much that it becomes difficult to quit, whereas another person would not experience such difficulty because they do not experience similar enjoyment from it as much as an addict would.
Neurological Sources of Addiction
Advances in neuroscience (science of the brain and nervous system) have provided a lot of support for the brain disease model of addiction. It has shown that people have varying levels of abilities and brain function to control impulsive urges with rational thought. Addicts sometimes also try to rationalise irrational acts or behaviours. You can find more information about that here.
Genetic Sources Of Addiction
Genetic factors can influence the severity of substance abuse. Approximately 50% of an individual’s likelihood to develop an addiction can be connected to genetic factors. Because of their genetic make-up, some people are more prone to the addiction than others.
Environmental sources
Environmental factors also contribute to the development of substance use disorder. High levels of stress, soldiers home after battles and war, childhood trauma, peer pressure, low parental involvement, bullying or abuse and many more, can all influence an individual to experiment with addictive substances. Studies show that early use of alcohol and/or drugs increases the chances of developing an addiction later in life.
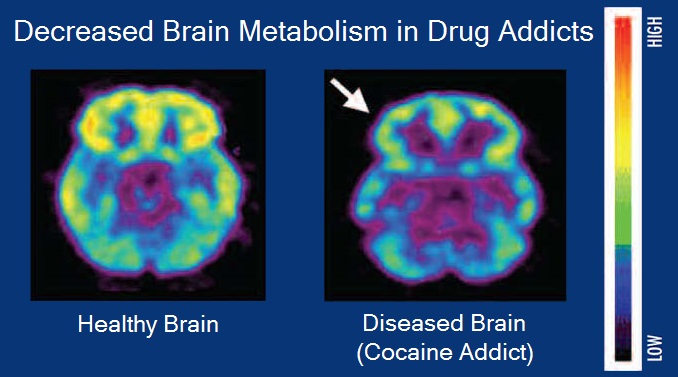
Classifying addiction as a brain disease
Most of the activities surrounding addiction takes place in the brain and affects it directly. Drug abuse induces changes in the brain’s structure and the way it functions. Over time, these changes, which are caused by the repeated process of abusing a substance, affect the user’s self-control and decision-making ability, whilst simultaneously sending impulses to take more of the drug or alcohol as the body stops producing its own chemicals as the rewards it gets from drugs and alcohol is a lot higher than the brain would ordinarily create, this then “entices” the person to go back for more and more.
Continuous exposure to a substance desensitises the reward pathways in the brain, thereby affecting the way the brain feels motivation and pleasure. The intensity and strength of conditioned responses are increased by the presence of the substance, which further leads to cravings as well as negative feelings when the substance is not taken or unavailable (dependence).
Upon cessation of drug or alcohol use, there are emotional reductions in the users/drinkers activity level, lack of motivational attitude towards getting into recovery and physical/psychological withdrawal symptoms. The brains region responsible for decision making, executive functioning, self-regulation and impulse control is weakened, thereby increasing the risk of relapse.
If you are currently going through a detox or withdrawal, you can find more ways to speed up this process and reduce the severity by adopting certain techniques. You can find out more about that here. Vitamins, minerals & supplements can also help, you can find information here.
How Substance Use Physically Changes The Brain
Chronic alcohol or drug use causes physical changes in the brain by creating long-lasting impairments to key functions and regions. These changes are responsible for establishing the brain disorder that makes substance abuse so difficult to discontinue using or drinking.
Drugs and alcohol bind to the receptor cells in the brain, leading to a release of certain neurotransmitters such as serotonin and dopamine, which in turn gives rise to an all-round feeling of relaxation, euphoria and pleasure. Once these substances enter the brain, the brain is less likely to produce its own. Because of this, the brain reduces its production of dopamine, serotonin and other neurochemicals, as they are being released unnaturally due to chronic, repetitive substance use.
This affects the receptors and the brain’s risk/reward system and the excess neurochemicals produced leads to tolerance and dependence and subsequent physical or psychological addiction to the substance. These processes change the physiology of the brain and it takes a significant amount of effort, therapy, treatments and recovery activities to get it back to its normal state.
Signs Of An Addiction
Here are some of the most common signs and symptoms addicts often display or present with, however this list is vast depending on particular substances, the amount you use or drink, your tolerance and many others.
- Alcohol or drug cravings
- Tolerance
- Emergence of withdrawal symptoms when the use of the substance is reduced or discontinued
- Failed attempts to quit the substance use
- Substance abuse interfering with obligations, commitments & responsibilities
- Withdrawal from activities previously enjoyed because of substance use
- Repetitive use of substance despite negative physical or social consequences
- Spending excessive amounts of time and resourcing in obtaining and using or drinking the substance
- Lack of money and possible debt
- Physical symptoms such as sweating, dilated or pin point pupils, slurring of words and others
Treatment Under The Disease Model Of Addiction
The disease model of addiction recognises that adequate treatment and therefore recovery and abstinence is possible and sustainable.
The treatment programmes largely depends on your exact needs, goals, how long you’ve taken drugs or alcohol, the amount, the frequency, whether you have been taking multiple substances at once, health conditions, mental health conditions and many other factors. Treatment facilities tend offer two types of programmes: outpatient (community based drug and alcohol services) and inpatient treatments (residential rehabilitation facilities). In inpatient treatment, patients live at a residential rehabilitation centre and detox full-time ranging from a few weeks to a few months and in some cases, years! In outpatient treatment, patients attend treatments and therapies in their own community, normally with a Keyworker and may also include MAT therapy too.
Research Into The Disease Model Of Addiction
Addiction is a disease affecting the incentive circuitry in the brain as related to motivation and pleasure. This then creating changes in behaviours, emotions and cognition. The debate over whether addiction is a medical disease or a mental health condition has led to much research and garnered many criticisms both for and against it.
Controversy About The Disease Model Of Addiction
There has been much controversy surrounding the idea that drug addiction is a disease. The criticisms are largely by those who subscribe to the life-process model of addiction. The life-process model of addiction is the opinion that addiction is a source of gratification and habitual response and not a disease. They believe that addiction shouldn’t be called a disease or disorder since the biological mechanisms that point to addictive behaviour have not been confirmed. They are of the opinion that an addict can defeat addiction through personal willpower, by repairing relationships, changing your behaviour or just stopping straight away.
Common Mental Health Conditions & Addiction
There are a few mental health conditions and behavioural disorders that tend to accompany addiction more commonly than some others. That’s why it is vital to treat every part of the addicts physical and mental health conditions and not simply isolate and treat their addiction alone. It’s important to never ignore the symptoms of a mental health condition when it comes to a person’s long-term addiction recovery plan.
Common mental health disorders commonly linked alongside substance abuse and addiction can include the following:
- Attention deficit hyperactivity disorder (ADHD)People with attention deficit hyperactivity disorder (ADHD) may be more inclined to abuse substances as a way to cope with their symptoms. Many people are prescribed stimulants to treat their ADHD, which can be habit-forming and lead to a toxic pattern of substance abuse
- Bipolar Disorder About half of people with bipolar disorder also struggle with addiction. As with any other disorder, it can be tempting to self-medicate to relieve symptoms. Drugs and alcohol provide a source of temporary relief from emotional situations and manic episodes for people with bipolar
- Borderline Personality Disorder Studies have shown that addiction and borderline personality disorder (BPD) often occur together. Over two-thirds of people with BPD have turned toward substance abuse at some point in their lives
- Depression An estimated one in 10 adults in the United Kingdom have reported suffering from depression. Many people diagnosed with depression try to self-medicate with drugs or alcohol. This often makes the problem worse although it may not seem that way at the time. The crash after the high can be devastating for those with a pre-existing depressive condition
- Eating Disorders Eating disorders often stem from strong feelings of inferiority or a negative self-image. Drugs that suppress appetite are especially common among people with these disorders
- Generalised Anxiety Disorder (GAD)The most common mental condition in the UK, generalised anxiety disorder (GAD) affects approximately 18-22 percent of the adult population. People who suffer from GAD may be more likely to abuse drugs and alcohol to manage and ease their intense symptoms. People may also abuse benzodiazepines, which are highly addictive prescription medications used to treat anxiety disorders
- Obsessive Compulsive Disorder (OCD) causes a number of unwanted obsessions and compulsions, such as an irrational fear of germs and the need to constantly clean. There are many variations of this illness. People with OCD often suffer from anxiety and depression as a result of their involuntary behavior, which can lead to substance abuse and addiction
- Post-traumatic stress disorder When a person develops post traumatic stress disorder (PTSD) their brain produces less endorphins than a healthy brain, making them more likely to turn toward alcohol or drugs to feel happy and function “normally” when flashbacks or other negative intense symptoms arise. According to the Ssafa, nearly 75% of soldiers and veterans who experience a traumatic or violent event during combat report repetitive alcohol or drug abuse
- Schizophrenia is characterised by hallucinations and delusional thinking. Diagnosing schizophrenia alongside an addiction can be difficult because both conditions share similar signs and symptoms. When a person has schizophrenia and uses substances as a way to self-medicate their condition, they risk putting their health further at risk

Why Co-Occurring Disorders Are Treated Differently
According to a recent UK wide survey, 45% of people in the United Kingdom struggle with a dual diagnosis. People diagnosed with a mental health condition are twice as likely to suffer from a substance abuse and addiction than the general population. Similarly, individuals who frequently abuse drugs or alcohol are likely to develop a co-occurring behavioural or mental health disorder. While it is widely accepted that a mental health disorder can induce a substance addiction – and vice versa – researchers are uncovering what causes both conditions to occur simultaneously.
A number of overlapping factors can aggravate a mental health or substance use disorder:
-
 Brain responses: abusing drugs can elicit symptoms that mimic a mental illness. For example, excessive marijuana use can give rise to psychosis in some individuals, which is a severe mental disorder that causes people to lose touch with reality.
Brain responses: abusing drugs can elicit symptoms that mimic a mental illness. For example, excessive marijuana use can give rise to psychosis in some individuals, which is a severe mental disorder that causes people to lose touch with reality.
 Genetics: A person’s genetic predisposition can make them more likely to develop an addiction or a mental disorder. Research shows that genes make up 40 to 60% of a person’s susceptibility to addiction.
Genetics: A person’s genetic predisposition can make them more likely to develop an addiction or a mental disorder. Research shows that genes make up 40 to 60% of a person’s susceptibility to addiction.
 Triggers: in the environment chronic stress, persistent anxiety or a traumatic event can kickstart an addiction or mental disorder.
Triggers: in the environment chronic stress, persistent anxiety or a traumatic event can kickstart an addiction or mental disorder.
- Exposure: at an early age people who experiment with drugs or alcohol at a young age may develop a substance abuse problem and/or mental health disorder later on. This is because adolescents and young adults are more prone to brain damage from substance use than older adults.
Warning Signs Of A Co-Occurring Disorder
The signs of a dual diagnosis vary greatly between individuals. Generally, symptoms will depend on the type of substance abused, as well as the severity of their co-occurring condition.
Symptoms Of A Dual Diagnosis Include:
- Sudden change in general behavior
- Difficulty managing daily tasks and responsibilities
- Avoiding events or social activities that were once enjoyed
- Neglecting health and hygiene
- Disillusioned thinking or cognitive impairments
- Refusal to seek or comply with treatment
- Mentions of thoughts of suicide or suicidal behaviours
- Erratic and impulsive behaviours
- Issues managing finances
- Poor performance at school or work
The Dangers Of Self-Medication & OTC Medicines
One of the most common issues surrounding dual diagnosis is self-medication. Self-medication involves using drugs or alcohol to mask the symptoms of a mental health illness. However, using substances as a coping mechanism for mental or behavioural illness can induce an addiction – and make the underlying mental condition even worse.
The following scenarios demonstrate how some people attempt to self-medicate a mental illness.
- Drinking alcohol to feel less anxious in social situations
- Taking excessive amounts of benzodiazepines (like Xanax or Valium) to ebb an oncoming panic attack
- Using marijuana to numb the emotional pain from trauma or grief
- Smoking or injecting cocaine to increase energy and motivation to complete daily tasks
- Smoking or injecting heroin to calm you down, get rid of pain or to just make you feel good
Sadly, resorting to substances as a way to escape a mental health condition can be a damaging decision. People struggling with a mental or behavioural illness who start abusing drugs or alcohol will consume as much as it takes to achieve the effects they want. Over time, the person will build a tolerance and need to consume more of the drug each time to achieve the same high. This negative, self-feeding cycle is what spawns a co-occurring substance addiction and mental health disorder.
Using over the counter (OTC) medicines can be just as addictive as illicit drugs if not use correctly, use it for longer than needed/recommended. Prescription medicines from your Doctor or GP can also be addictive. Don’t assume that because it comes from your Doctor, that you can’t become addicted or that they cannot be abused (using when not needed for prescribing condition, to make you feel good or give to someone else).
Don’t Let Covid-19 Stop You from Getting Help

Your local drug and alcohol service and residential rehab facility are still open and able to help you with your addiction. If you feel ready for help, you can find contact information for charities, organisations and groups, who can help you on our help & support page here.
Get Help For A Dual Diagnosis

The image above will give you a few rough ideas as to how you can help your mental health and addiction during lockdown & Covid-19. If you need more support, help or advice, you can find contact information for various organisations and charities who can help. You can find our help & support page here.
While some individuals develop an addiction to drugs or alcohol before being diagnosed with a mental disorder, others become addicted after acquiring a mental disorder. Whichever happened first, it’s paramount to find a tailored treatment plan that targets both disorders simultaneously – rather than a plan that treats them separately. In the case of a dual diagnosis, the best form of treatment is a your local community based drug and alcohol service or in the structured, safe environment of an inpatient rehab centre. They are both able to help you, its up to you which you feel would be most appropriate for you. Due to covid-19, certain facilities at residential rehabilitation facilities may not be able to offer you a full program as they otherwise would normally. We recommend you contact your local community drug and alcohol service first, as they can get help and treatment started straight away, where as a rehab may take a little longer.
Going to inpatient rehab for a co-occurring disorder is ideal because of the high level of attention and care that patients receive. Oftentimes, people with co-occurring disorders arrive at rehab in various states of distress and poor general health. The combination of extensive substance abuse and a neglected mental condition generally requires the help of both mental health and addiction professionals.
Community based drug and alcohol services are able to offer you talking therapies, group therapies (online at present due to covid-19), MAT programs and many more.
If you feel you need help for your drug use or drinking and feel ready to make a change in your life, you can find contact information on our help and support page here for organisations, charities and group who can help!


7 thoughts on “Mental Health And Addiction – Why The Two Often Go Hand In Hand”